Isabelle Racine-Miousse, PhD
Assistant Professor
Biochemistry
College of Medicine
University of Arkansas for Medical Sciences
Thematic Area: Methionine and Epigenetics
Nearly 10,000 Americans die from melanoma every year. Since 2011, immune checkpoint inhibitors have been approved for metastatic melanoma. These antibodies enhance a person’s immune system’s ability to recognize cancer cells. Despite a major improvement in remission rates, the majority of patients do not respond to immune checkpoint inhibitors. The identification of approaches to overcome immune checkpoint inhibitor resistance, as well as new therapeutic strategies to treat metastatic melanoma, are crucially needed.
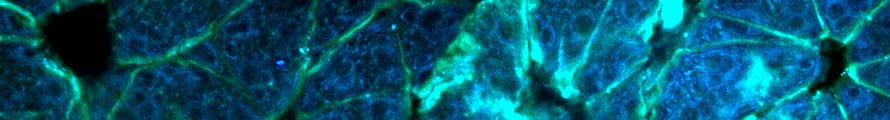
Cancer cells rely on exogenous sources of methionine, contrarily to normal cells that can thrive off the remethylation of homocysteine. Our data shows that at levels that maintain body weight, a methionine restricted diet dramatically reduces tumor size and number of lung metastases in an immunocompetent murine melanoma model. Our preliminary data indicates that the effect involves mitochondrial function. Recent work highlighted the importance of mitochondrial function in immune checkpoint inhibitor responders versus nonresponders. The combination of methionine restriction and immune checkpoint inhibitor responsiveness has never been tested.
In addition to direct effects on methionine dependent cancer cells, we have determined that alterations in dietary methionine affect the gut microbiome. It is now well-established that there are significant differences in the gut microbiomes of patients with metastatic melanoma that are associated with efficacy of immune checkpoint inhibitor therapy, and that responsiveness can be induced with fecal transplantation in animal models. However, the impact of a methionine-regulated microbiome on melanoma growth, metastasis, and immune checkpoint inhibitor responsiveness is unknown.
According to our data and supporting scientific literature, we hypothesize that dietary methionine restriction will promote antitumor mechanisms, including autophagy and microbiome alterations, which will increase immune checkpoint inhibitor responsiveness for metastatic melanoma. To test this hypothesis, we propose to study the effect of a methionine restricted diet in a preclinical, immunocompetent mouse model of melanoma. Following establishment of tumor, mice will receive a standard diet or an identical diet containing low levels of methionine to investigate the following:
- Determine whether methionine restriction increases responsiveness to immune checkpoint blockade in a preclinical mouse model.
- Determine the contribution of gut microbiota in methionine-dependent antitumor activity.
Our study investigates a novel approach to decrease mortality due to metastatic melanoma. We expect the results generated from our studies to be translatable to other types of malignancies, especially those for which immune checkpoint inhibitors are used for therapy.